What Is Lupus?
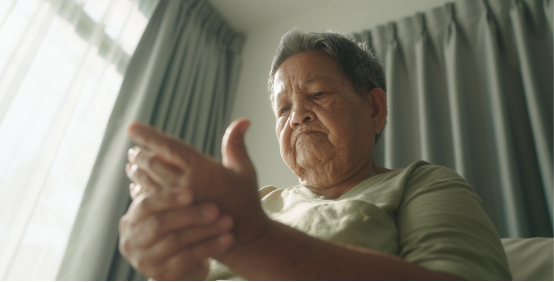
Lupus is a chronic disease with a variety of symptoms caused by inflammation in one or more parts of the body. It is estimated that it affects over 1:1000 Canadians.
Who gets lupus? Anyone can: women, men, children. Between the ages 15 and 45, eight times more women than men get lupus. In those under 15 and over 45, both sexes are affected equally.
Lupus is not contagious and is not related to AIDS or cancer. It belongs in the family of diseases that includes rheumatoid arthritis, multiple sclerosis, juvenile diabetes, and scleroderma.
Did you know:
Are There Different Types?
Yes, there are 4 kinds of lupus.
When people talk about lupus, they’re usually talking about systemic lupus (SLE). But there are other types of lupus which mainly affect the skin. A few individuals develop drug-induced lupus as a response to some medications used to treat other conditions. These symptoms disappear when the person stops taking the medication.
- Discord lupus erythematosus & subacute cutaneous lupus
- Neonatal lupus
- Drug-induced lupus
- Systemic lupus erythematosus
The different types of lupus:
Discoid lupus erythematosus (DLE) & subacute cutaneous lupus (SCLE)
Neonatal lupus
Drug-induced lupus
Systemic lupus erythematosus SLE
Who Can Get Lupus?
Anyone can: women, men, children.
Fact Check:

Is lupus hereditary?
There is a possibility of having lupus if a family member has an auto-immune disease or lupus.
It is not unusual for a lupus patient to have in his or her family a relative with an autoimmune disease (including lupus). In fact, SLE studies have shown that between 0.4 to 5 percent of the relatives of lupus patients may themselves develop lupus. While this may sound frightening, remember that the odds of not having lupus when someone else in the family has it are at least 95 percent or greater.
Is there a cure?
Currently there is only treatment.
How does lupus affect life expectancy?
With earlier diagnosis, life expectancy is showing remarkable improvements.

Still have questions?
Read our lupus FAQ or get your Intro Guide to Lupus Booklet.

Hopeful facts about systemic lupus erythematosus (SLE)


Better methods of diagnosis, treatment and follow-up have improved the life expectancy of lupus patients so that nowadays, lupus is seldom seen to be fatal.

Many patients undergo cycles in which the disease becomes quiet after it is brought under control. This symptom-free period is called remission and may last several years.

Lupus is treatable, and much can be done to control it. In fact, with proper treatment, it is the rule, not the exception, for physicians (and patients) to succeed in bringing lupus under control.

Lupus can be a serious disease, but it is quite clear that milder forms of the disease do exist and are being increasingly recognized.
A brief history of lupus
Lupus has been known as a disease for over 2000 years. Hippocrates, who lived from 460 to 370 BC, first described lupus lesions (lesions means damage). The name “lupus” comes from a Latin word meaning wolf and was used in reference to the ulcers on the face. In 1851, Cazenave introduced the name “ lupus erythematosus. ”
Later in the 1800s, Kaposi described the butterfly rash on the face, and Sir William Osler, a Canadian physician, expanded the concept of lupus as a “ systemic ” disease, a disease which may affect many parts of the body.